Flatback Syndrome: When a “Straight” Spine is Abnormal
There are several natural curvatures along the human spine. Sometimes—for one reason or another—this curvature can undergo an abnormal change. One such common condition comes in the form of what experts call “flatback syndrome.”
With flatback syndrome, the natural curvature of the lumbar spine becomes imbalanced. When you look at a cross-section of the human spine from the side, it appears to be in an “S” shape. In this instance, the lower part of the “S” becomes straight, which leads to a slew of other problems for the people with this condition.
The main concern with this is that it misaligns the patient’s center of gravity. The “S” curve minimizes the toll that gravity that takes on the body, and both of the spinal curves cancel each other out to provide stability. When one of these curves misaligns, this balance is disrupted.
It may sound strange, but the reality is that you really don’t want your lumbar spine to be perfectly straight. It’s supposed to be curved. When the lumbar spine loses its curvature, it causes chronic pain, as well as difficulty standing and performing everyday tasks. Even worse, a person with this condition often has to overcompensate by using muscles in other areas of the body to stand upright. These compensatory changes may give the patient relief for the time; but, eventually, this will just exacerbate the problem.

Symptoms of Flatback Syndrome
Again, the main symptoms of flatback syndrome include difficulty standing upright and pain in the lumbar region of the patient’s back. That being said, pain may also occur in the thigh and groin areas as well. Usually, patients with this condition find that their symptoms worsen as they go about their day. This is partially due to the fact that the body overcompensates for the spinal abnormality, leading to excess fatigue and difficulty maintaining proper posture. Additionally, many patients also flex at the knees and hips, to help maintain a correct standing posture. As the day goes on, these compensatory changes just wear the body down as the muscles in those regions exhaust their resources.
The symptoms don’t just end there, though. In some cases, a person with flatback syndrome may also show signs of spinal stenosis as well as sciatica. Furthermore, sometimes, the pain doesn’t just begin and end with the lumbar spine. A portion of patients with flatback syndrome note a degree of chronic pain in the cervical spine and upper back area. Over time, these symptoms may handicap the patient, leading them to require prescription pain meds as well as limiting their daily routine.
What Causes Flatback Syndrome?
In the past, there have been correlations between flatback syndrome and patients who have had spinal treatments involving Harrington rods. This instrumentation was one of the first spinal implants invented, and originally, doctors used it to treat scoliosis of the spine. Unfortunately, Harrington rods would often straighten out or “flatten” the lumbar spine. This is especially so if the doctor implemented the rods to treat scoliosis in the L4/L5 region of the area.
Of course, this is now a bygone system. Doctors routinely used Harrington rods to treat spinal conditions in the 60s, 70s, and 80s. Since that time, medical experts have modernized spinal implements that no longer cause such problems. This isn’t to say that Harrington rods did not have any benefits, however. In fact, patients who were given Harrington implants as treatment typically did well for the first few decades. But, over time, the discs below the fusion area degenerated, which led to chronic pain and an inability to maintain a good standing posture.

Other Known Causes of Flatback Syndrome
Harrington rods are not the sole cause of flatback syndrome, however. In fact, there are several conditions that may lead to the development of this condition. Common causes of flatback syndrome include:
- Ankylosing Spondylitis: An arthritic spine disease that causes lumbar stiffness, and on occasion, flatback syndrome.
- Degenerative Disc Disease: Somewhat of a blanket term that describes spinal structures that wear down because of normal age-related wear and tear. Affected discs will often contribute to spinal stiffness in the lumbar region, leading to flatback syndrome in susceptible individuals. Patients with this problem have difficulty standing upright. And, this only gets worse with time.
- Vertebral Compression Fractures: This condition describes a scenario in which the front portion of a patient’s vertebra collapses. Usually, this happens when the patient has been diagnosed with osteoporosis. This structural weakness can result in flatback syndrome if enough vertebrae are compromised.
- Post Laminectomy Syndrome: A subset of the failed back surgery syndrome category. Some patients find that after having a lumbar laminectomy, they notice a negative change in stability as well as a loss of lumbar lordosis.
These are just to name a few causes. As with anything medical, a lot can potentially go wrong. So, the list technically spans for miles.
How is Flatback Syndrome Treated?
Most medical conditions have two categories of treatments available: surgical and non-surgical. Of course, this is not universally true, but for most cases, it rings true. Flatback syndrome is simply not an exception. Usually, doctors will try to exhaust the most conservative treatment options first. For flatback syndrome, these include:
- Physical Therapy
- Steroid Injections
- Pain Medications
- Conditioning & Exercise Programs
- …and more.
Surgical Procedures for Flatback Syndrome
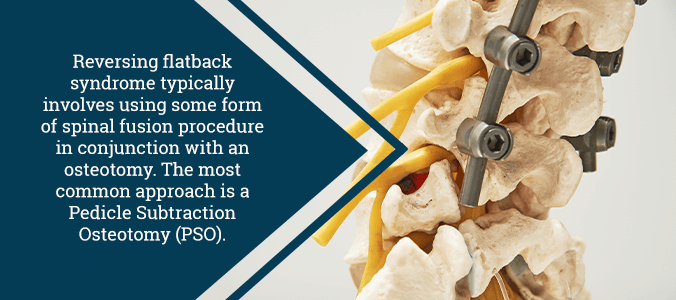
As for surgical treatments, doctors most commonly perform a Pedicle Subtraction Osteotomy (PSO) to remedy flatback syndrome. This procedure works on both children and adults to correct certain abnormalities within the structures of the spine.
A doctor performs this procedure under general anesthesia. To protect the nerve endings of the spine, doctors will often read somatosensory evoked potentials and motor-evoked potentials while performing the surgery. These monitoring techniques measure neural activity and they give the performing doctor an idea of the spine’s condition in real time.
After the patient goes under, the doctor then carefully places them face-down on a special type of operating table. Next comes the placement of the rods and screws. The surgeon begins by placing screws into the pedicle (the bone that connects the front of the vertebrae to the back of the spine). These screws will provide useful attachment points for the rods that the doctor will add later.
Next, the surgeon removes the processes (bony projections on the backside of the vertebrae) from the affected area. The surgeon then removes the pedicles to create more space, leaving a wedge-shaped hole in the vertebrae. Using their specialized table to adjust the patient’s position, the surgeon will close this wedge, adjusting the curvature of the spine.
Lastly, the doctor will apply the rods to the screws that were inserted earlier. These will help the spine hold its position during the recovery period. Eventually, the bony surfaces in the area will fuse together into a single strip of solid bone.
Dr. Jason Lowenstein: Flatback Syndrome Specialist
Do you have flatback syndrome resulting from a medical condition or failed back surgery syndrome? If so, contact us today at (855) 220-5966. Dr. Jason E. Lowenstein is one of the industry’s best specialists in spinal deformity diagnostics and treatment. He is well-known as a founding member of the Advanced Spine Center, while also serving as the medical director of spinal deformity at Morristown Medical Center. Don’t let your medical condition dictate your life. Get the relief you deserve today!
