Flatback Syndrome after Harrington Rod
Revision Scoliosis Case
This is a 55 year woman who presented with progressive worsening back pain and inability to stand up straight. She underwent a Harrington Rod surgery as a child for treatment of Scoliosis. In adulthood, she began developing lower back pain, and the pain would travel into her buttocks and thighs, along with numbness and tingling. Over time she developed increasing difficulty standing up straight.
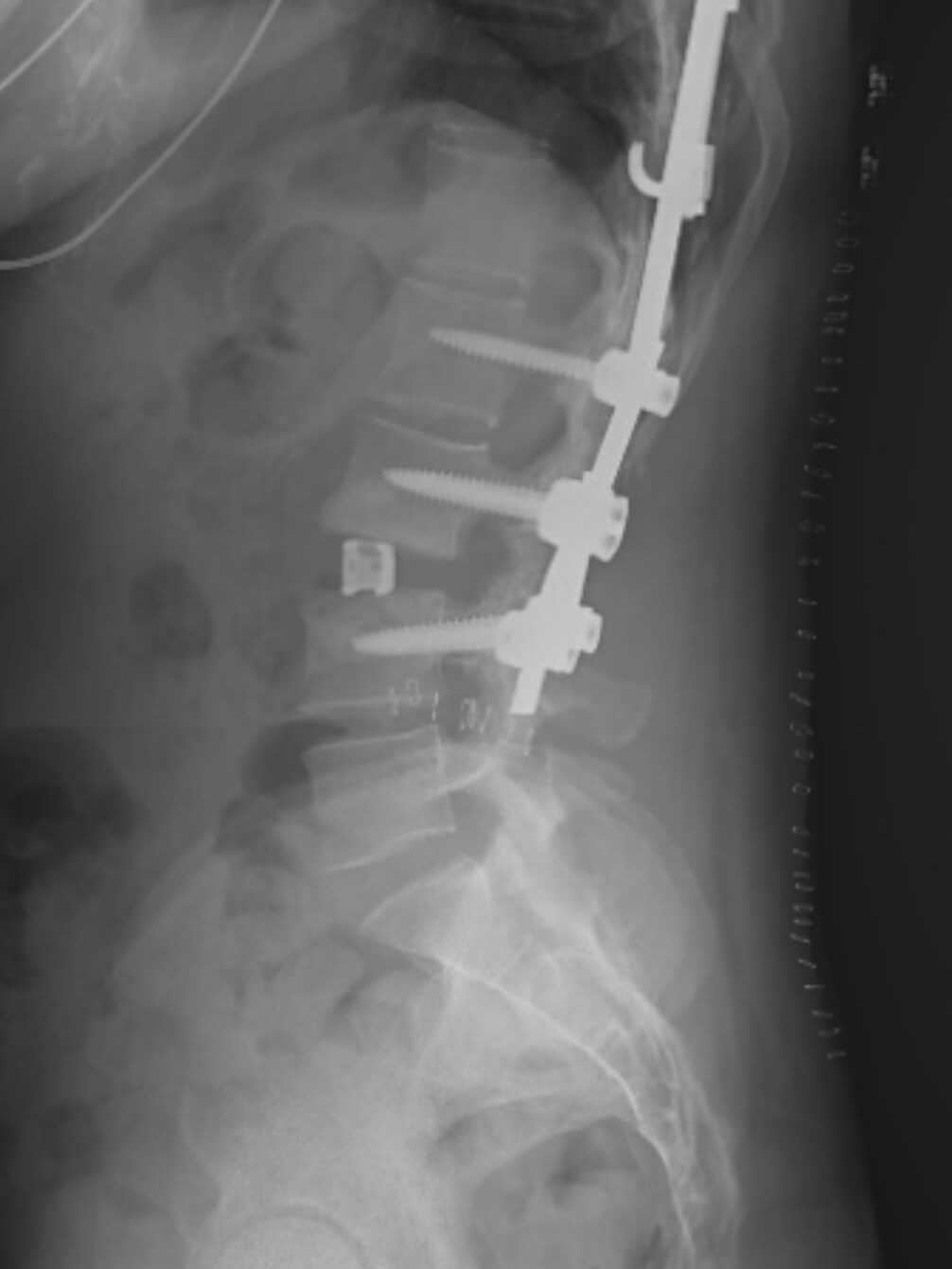
Her X-rays show her Harrington Rod instrumentation, starting at T5 and extending down to L3. Her lateral x-rays (from the side) show severe disc degeneration at L3-4, the motion segment directly below her fusion, with kyphosis, or angling of the disc space in the forward direction, confirming her diagnosis of Flatback Syndrome.
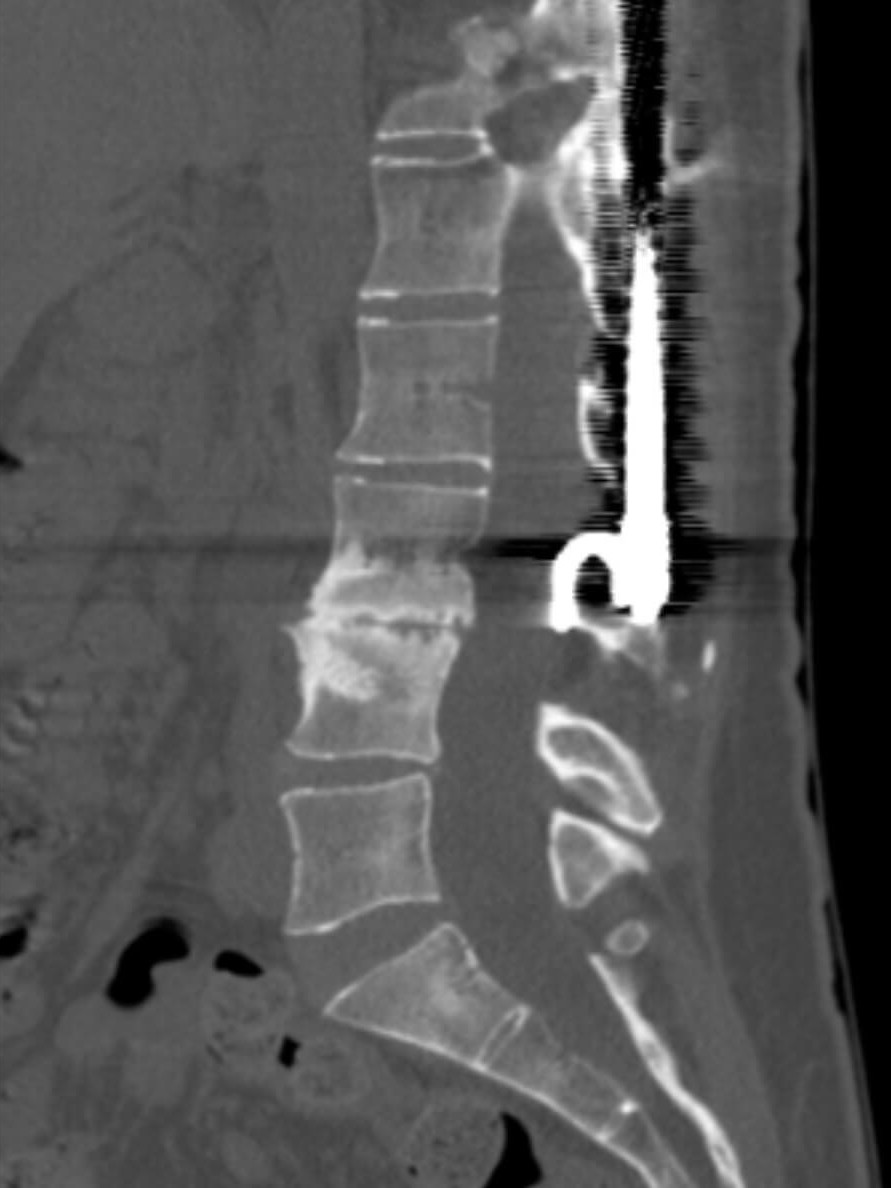
Her CT and MRI further illustrate the severe degenerative disc disease at L3-4, the level directly below her fusion, with “auto-fusion” or bony bridging across the L3-4 disc space.
Treatment
Because of her severe flatback syndrome and progressive symptoms that were not improved with conservative treatment strategies, such as physical therapy, oral pain medications, and pain management with epidural steroids, she was a candidate for revision spine surgery. The goal of the surgery was to open the disc space at L3-4 to regain the height of the disc that she lost, or restore her lordosis, to help her mechanical back pain and allow her to stand up straight, but also to take the pressure off her nerves that were being compressed at L3-4.
She first underwent a minimally invasive, lateral surgery to address the disc collapse at L3-4. This was achieved using a newer technique called a “Prone Transpsoas Surgery”, where the patient is positioned lying prone, or on their stomach, and both the anterior spine and posterior spine can both be surgically approached in this singular position (saving time during surgery and allowing for better deformity correction.) An osteotomy was done at the L3-4 disc, cutting the bridging bone that had grown across the disc space allowing the disc to be released, or opened, to allow regain the height that had been lost as the disc collapsed over time. A cage, or metallic spacer, was placed into the disc space to maintain the restored disc space height. This was then followed by the posterior surgery, where the distal Harrington Rod hook was removed to allow for decompression of the spinal stenosis at L3-4, along with placement of additional spine hardware (pedicle screws) from L2-4 to further stabilize the spine in its corrected position, addressing both her flatback syndrome and recurrent spinal stenosis. She had immediate improvement in her back and leg pain, was able to stand up straight, and went on to have an excellent clinical outcome.