Failed Back Surgery Syndrome
What Is Failed Back Surgery Syndrome (FBSS)?
For most patients, undergoing spine surgery will alleviate a slew of debilitating symptoms that interfere with day-to-day functioning. Unfortunately, however, this is not always the result of such procedures. Sometimes, things go wrong—or more accurately—they fail to achieve the desired results.
Doctors often refer to the resulting symptoms of an unsuccessful back surgery as Failed Back Surgery Syndrome (FBSS). In this instance, the patient had a condition that was deemed viable for surgical treatment and has undergone such a treatment. Unfortunately, after the operation has been performed, pain from their original condition persisted. The surgery was a failure so to speak.
The spine is a vastly complex network of interconnected bones, nerves, joints, and other tissues. It is the neural Autobahn of traveling information within the body. Abnormalities within this microcosm may lead to problems in seemingly unrelated areas of the body. Sometimes, problems within the spine show absolutely no perceivable or negative symptoms in the patient. Because of these facts, it is understandable how easily things may go awry. Even the most skilled specialists cannot guarantee the success of a given procedure. In fact, it is believed that any given spine surgery cannot have a predictive success rate higher than 95%. The reason for this traces back to the complexity of the spine. Believe it or not, the most common cause of FBSS is not surgeon error, although this does occur. Instead, it is usually because the treated area was not actually the cause of the negative symptoms.
The most common symptoms of FBSS are the following:
- Pain: The most common symptom, pain, manifests in a variety of ways. Additionally, because the spine has so many branching nerve roots, this pain may occur in seemingly unrelated areas. The most common examples involve the arms and legs. This pain may be dull and persistent, or it may be sharp and acute.
- Neurological Symptoms: As mentioned earlier, complications may lead to conditions such as quadriplegia or total paraplegia. And, these conditions can lead to paralysis in the arms and/or legs. In other cases, different sensations may appear. A common example of this is a pins-and-needles tingling sensation experienced in different parts of the body. Also, in some sciatica cases, the patient may achieve pain relief, but still have muscle spasms.
- Additional Abnormalities: After a failed spine surgery procedure, you may develop other conditions. These other conditions can range widely in symptoms and severity. Commonly cited examples include recurrent disc herniation and the crankshaft phenomenon. Usually, however, the former is more common than the latter. It is important to note that disc herniation may develop independently after a failed spine surgery. These two phenomena do not necessarily have to correlate.
How Do I Know If I Have The Symptoms of FBSS?
There are many different reasons that might classify a surgery as a failure. For instance, it may simply be that the procedure doesn’t relieve the patient’s initial condition. Aside from that, a doctor may consider a surgery a failure if it leads to an additional spine condition or other complications.
If you still have symptoms or develop new ones after a spine surgery procedure, please contact Jason E. Lowenstein at 973-538-0900. Jason E. Lowenstein is a highly specialized, fellowship-trained spinal deformity surgeon. Using the latest methods in both conservative and minimally invasive procedures, Dr. Lowenstein will find the best treatment plan for you.
Fusion Surgery & Failed Back Surgery Syndrome
Spinal fusion is one of the most common surgical procedures that doctors use to treat a myriad of abnormalities, including spinal deformities. Most often, a doctor performs this technique to treat both pediatric and adult scoliosis, as well as recurrent disc herniation. The goal of fusion surgery is to fuse two or more vertebrae together, increasing stability and reducing pain. This technique is especially effective in addressing scoliosis, as spinal fusion can actually reverse the lateral curvature of the spine. Sometimes, spinal fusion may even be used to help heal broken vertebra.
Spinal fusion is a popular treatment for good reason: it effectively provides pain relief and it usually works. However, as mentioned previously, there is no spinal procedure that guarantees 100% success. For spinal fusion, there is a perceivable correlation between the solidity of the fusion and positive results. While this may be, it is still possible for the patient to achieve relief even if the fusion is not solid. This result usually arises when the surgical hardware remains intact and the spinal stability is still good. Considering the goal of spinal fusion, this makes a fair bit of sense. Remember, the priority is not necessarily achieving a solid fusion. Instead, it is most important that the procedure achieves spinal stability.
Interestingly enough, spinal fusion becomes more complicated after the procedure has been performed. In most cases, it is not easy to immediately tell if the fusion was successful. In fact, it may take anywhere from three months to one year to achieve a solid fusion. Because of this problem, some surgeons may not even consider further surgery if a year has not yet passed. Unless there are observable structural or hardware failures, surgeons will not perform further procedures until the spinal fusion recovery period is over. Thus, FBSS is difficult to detect for fusion.
Harrington Rods
During the early 1960s all the way up to the 1990s, doctors often used Harrington rods to treat scoliosis symptoms via fusion. Today, most surgeons only recommend Harrington rods for a Cobb angle greater than 45 degrees. Additionally, children with scoliosis are almost never viable candidates for these rods. This is because young children still have growing to do and Harrington rods are incredibly difficult to replace. In immature skeletons, Harrington rods may lead to an angular spinal deformity known as the crankshaft phenomenon. This is primarily why these rods are avoided in pediatric cases, as this condition has limited treatment options.
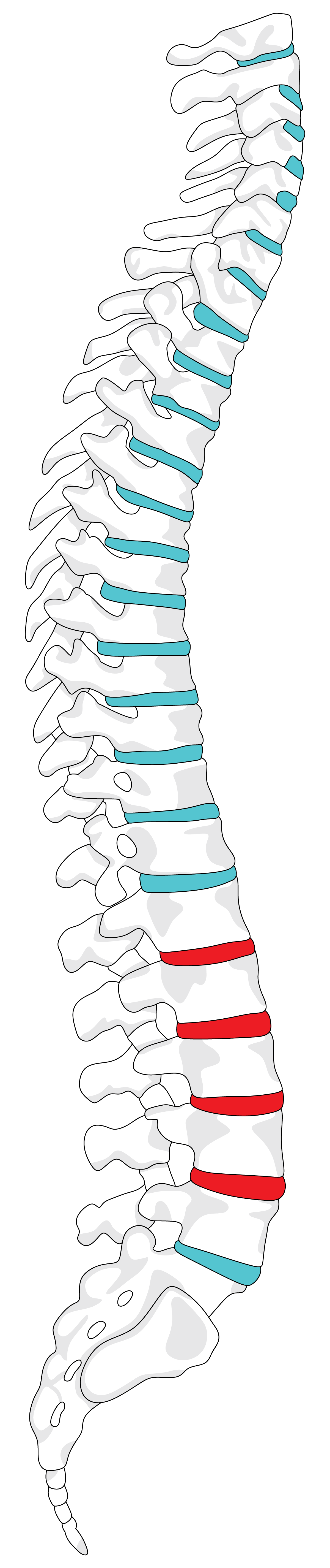
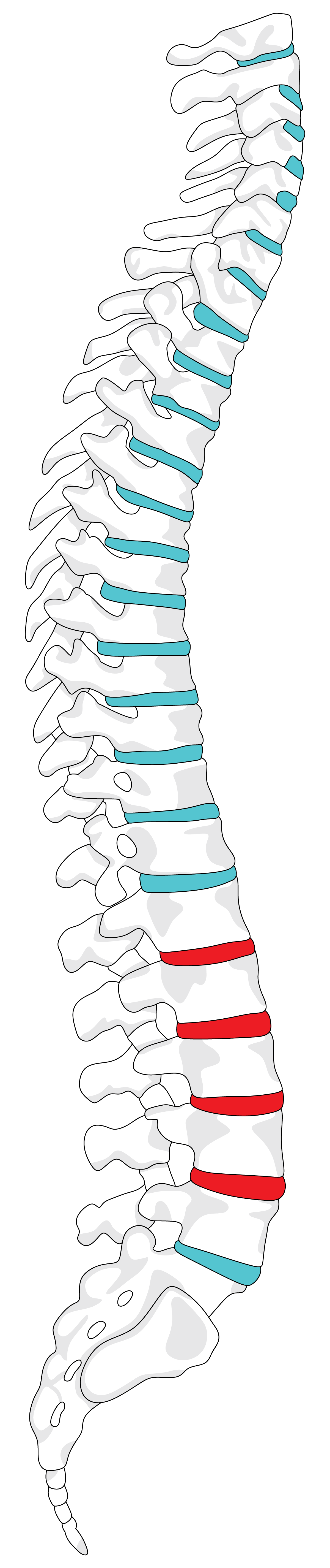
Harrington rods are incredibly invasive, so the potential complications can get pretty severe. Aside from simply failing to relieve pain, there are additional risks layered on top. For one, many traditional open spinal surgeries carry the risk of total paraplegia or even quadriplegia. In some cases, Harrington rods may even lead to a condition known as flatback syndrome. This occurs in cases where the rods were used in the lumbar region of the spine. In this region, Harrington rods do not physically agree with the natural curve of the spine. As a result, the spine may straighten into an unnatural position. At first, this may seem inconsequential, but it often leads to the degeneration of structures within the spine.
Spinal Stenosis Surgery Failure
Spinal stenosis is a common back abnormality as it often occurs naturally through age-related wear and tear on the spine. Surrounding the spine is a network of passageways through which nerves branch off and exit. When these passageways narrow (usually because of an underlying condition or aging), it puts pressure on these exiting nerves. This, in a nutshell, is how spinal stenosis occurs. The patient may experience no symptoms, or they may feel varying degrees of pain. This mostly depends on whether or not there are pinched nerve roots.
In more severe cases of spinal stenosis, a doctor may recommend a laminectomy (a form of spinal stenosis surgery). For this procedure, a surgeon removes the patient’s lamina (the backside of the vertebra). This creates more space in the affected area(s), which in turn relieves the pressure that spinal stenosis places on the spinal cord.
Much like with fusions, the success of a laminectomy is hard to measure immediately after the procedure. Again, there is often a three-month grace period before observable results are even detectable. Eighty to ninety percent of these decompression surgeries prove to be successful. In the remaining minority, the surgery does not relieve pain or leads to recurrent disc herniation. In such instances, your doctor may recommend an additional procedure, such as revision spine surgery.
How Dr. Lowenstein Can Help
There are both conservative and minimally invasive surgical treatment options for patients who suffer from FBSS. Usually, orthopedic surgeons exhaust conservative treatments first and only opt for surgery if absolutely necessary. In more severe cases, doctors may skip this initial step and immediately recommend revision spine surgery. This may include an additional spinal fusion or a facet joint rhizotomy, depending upon your unique case. It is important to communicate your symptoms with your doctor to receive the best possible treatment.
Examples of conservative treatment include:
-
- Physical therapy
- Nerve block injections
- Pain medication (usually over the counter or prescription NSAIDs)
- Medically advised exercises
- Heat application to the sore areas
- Acupuncture
Dr. Jason Lowenstein, spinal deformity and scoliosis doctor, is here to help you return to a normal, functioning lifestyle. His team of revision spine surgery experts will work tirelessly to provide you with the best pain management and treatment plan for you. To schedule an appointment or for general information, contact our practice today!